Gallery
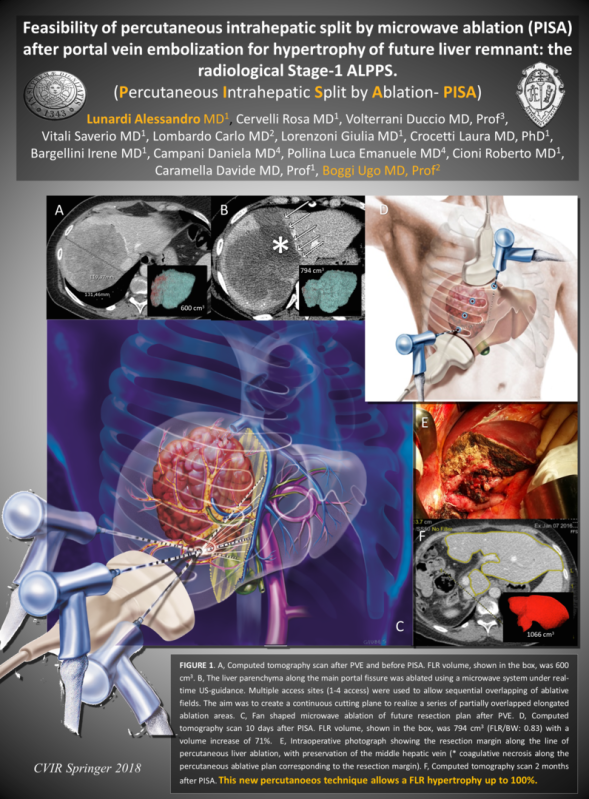
SPLIT EPATICO PERCUTANEO - P.I.S.A.
Articolo in Stampa su Cardiovascular and Interventional Radiology (CVIR 2018)
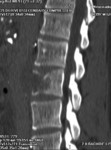
TECNICA DI SPLIT EPATICO PERCUTANEO ECOGUIDATO
"PISA"
1 settimana dopo l'embolizzazione portale il fegato viene diviso seguendo il futuro piano chirurgico con un taglio ablativo percutaneo mediante microonde. Il paziente deambula
dopo poche ore dall'intervento che viene effettuato in sedazione profonda.
Il fegato sano raggiungerà volumi superiori al 100% del volume iniziale (63-110%) permettendo al chirurgo di effettuare l'epatectomia maggiore con un minor rischio
di insufficienza epatica post-operatoria.
Questa tecnica innovativa è stata ideata
dal Dott. Alessandro Lunardi assieme al Prof. Ugo Boggi nel 2015.
CVIR 2018 Springer: http://rdcu.be/Fmot
Primo intervento di "P.I.S.A." effettuato dal Dott. Lunardi nel 2015
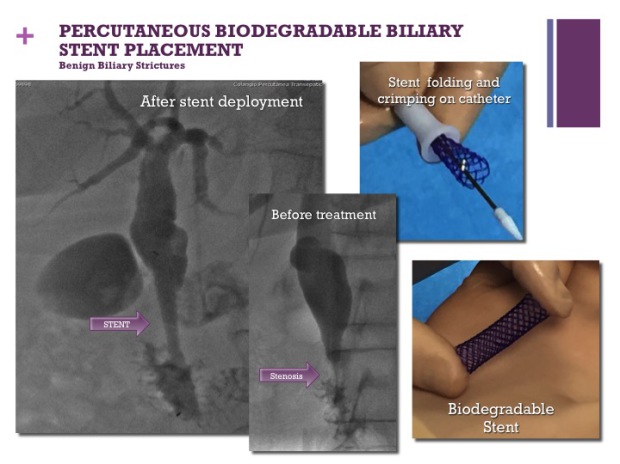
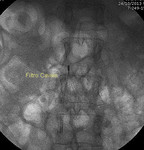
INTERVENTISTICA BILIARE PERCUTANEA
TECNICA MININVASIVA
Puntura ecoguidata della Via Biliare - Radiologia Interventistica
Interventistica Biliare Pecutanea - Radiologia Interventistica
Accessi mininvasivi - Radiologia Interventistica
Drenaggio Biliare - Radiologia Interventistica
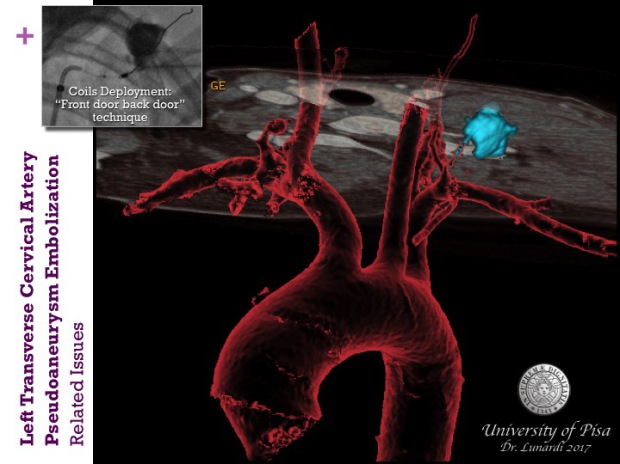
This young female patient developed a left transverse cervical artery pseudoaneurysm after the unsuccessful attempt of ipsilateral Internal Jugular vein catheterization during the hospital stay for orthotopic liver transplantation.
PHOTOS GALLERY